Global Disparities in Treating Multimorbidities
By: Neha Bajaj
In the twenty-first century, access to high-quality medical treatment depends on the socioeconomic status of a country. The higher the developmental status, the greater quality of medical treatment a citizen may expect to receive. This relationship can be used to analyze how multimorbidity treatment varies across the globe. Multimorbidities are defined as the coexistence of two or more chronic health conditions in an individual. To determine the global disparities that exist in treating multimorbidities, this paper compares multimorbidity data and typical treatment mechanisms from three countries in various stages of socio-economic development: the United States, Nepal, and Africa.
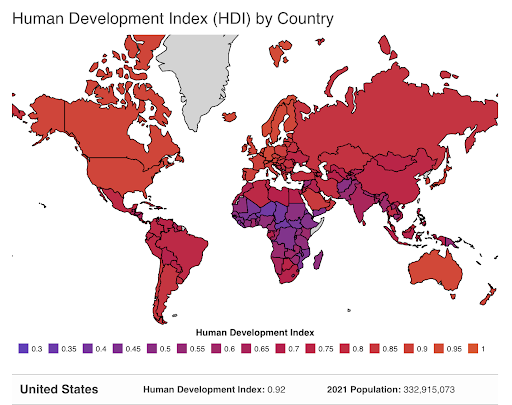
The 2020 Human Development Index (HDI) was chosen to be the indicator for each country’s developmental status because it employs key human development assessors such as life expectancy, standard of living, etc. Compared to other research measurements, the 2020 HDI demonstrates a comprehensive review of a nation’s achievement and can be accurately used to compare the developmental status of countries around the world.
The United States earns a HDI score of 0.926 out of 1 which indicates a high human development. More specifically, this number reveals that the U.S. has “healthcare and a high life [expectancy]” (Human Development Reports, 2020). However, despite these advancements, there is still a large portion of multimorbidities that exist within the US population. Currently, more than one-quarter of American adults are diagnosed with multiple chronic diseases, most commonly hypertension and arthritis.
Figure 1. 2020 Human Development Index variations from across the globe.
To treat multimorbid patients, the U.S. healthcare system utilizes polypharmacy, the usage of more than one drug by a single patient for more than one condition. While each medication prescribed treats one of the chronic conditions that a patient is facing, this increase in medication can potentially result in lethal synergistic reactions in the patient. Due to the vast resources available to the country, the US can utilize complex pharmaceutical techniques to treat multimorbid patients. As such, the high socioeconomic level of the US is indicative of the treatment options available to American citizens with multimorbidities.
Nepal earns an HDI score of 0.602 out of 1 which lies below the threshold for a ‘developed’ country (0.8 and above), yet above the cutoff for an ‘underdeveloped’ country (0.55 and below). In terms of healthcare, Nepal maintains an “unequal distribution of health care services and an inadequate supply of essential drugs” with only “0.67 doctors and nurses per 1,000 [people]” (Mishra, 2015). To determine the prevalence of multimorbidities in the older Nepalese population, 794 Nepalese older adults were recruited in 2018 by the Forum for Health Research and Development. Data from the study found that 48.9% of the participants had at least one chronic condition and 14% were multimorbid. These statistics can be translated to the greater Neaplese adult population to indicate that a large proportion of citizens have multimorbidities, most commonly Osteoarthritis and Chronic Obstructive Pulmonary Diseases.
Figure 2. The most prevalent multimorbidities in Nepal from a cross-sectional study by the Forum for Health Research and Development for 794 Nepalese adults.
In order to treat these conditions, Nepalese medical services focus on treating patients with services available to them from solely tertiary healthcare systems, clinics with higher level specialized care. These healthcare systems are typically the only treatment options available to patients as primary clinics do not have the capacity nor resources to address the needs of those with multiple chronic conditions. From this, Nepal focuses on an “integrated primary care approach when treating pre-existing non-communicable chronic conditions” (Yadav, 2021). In comparison to the USA, Nepal does not follow the approach of prescribing pharmaceuticals, but instead utilizes different sectors of healthcare to produce treatment plans.
Furthermore, the Central African Republic earns a score of 0.397 out of 1 on the HDI effectively classifying it as a least developed country characterized by a “poor education and a lack of access to healthcare” with “low life expectancies and high birth rates” (Human Development Reports, 2020). In a study conducted by the INDEPTH Community in South Africa Programme, a population of 3,889 were enrolled to determine the amount of chronic conditions that exist within the study population. The data indicated that “69.4% of the respondents had at least two chronic conditions” with the most common multimorbidities being cardiometabolic conditions and HIV (Chang, 2018). The medical treatment for multimorbid patients in the Central African Republic are synergies which is an approach used when medical treatments are “bundled together to facilitate a better quality of care” (Chang, 2018). In comparison to the USA’s treatment, synergies are similar to polypharmacy as they both involve the combination of medications or treatments for optimal care. However, the Central African Republic’s treatment is different from that of Nepal’s as they do not utilize a multi-sectoral treatment approach.
Figure 3. Proportion of citizens with multimorbidities in the Central African Republic categorized by gender and number of multimorbidities from the INDEPTH Community in the South Africa Programme.
Overall, from the multimorbidity data of the USA, Nepal, and the Central African Republic, it can be concluded that there is no strong correlation between the socioeconomic status of a country and the amount of multimorbidities present within that country.
Although the USA is considered highly developed, there is no indication that there are low levels of multimorbidities in the US in comparison to the Central African Republic which experiences high multimorbidity rates and a lower developmental status. In addition, medical disparities exist with the treatment of multimorbidities between the three countries. The USA follows polypharmacy while Nepal relies mostly on a multi-sectoral care approach. The Central African Republic then mostly follows synergic treatments. In conclusion, this data is relevant to global health as it establishes the stark differences that exist in treating multimorbidities across the varying developmental statuses of countries. The understanding of global disparities is pivotal to ensuring equal health status and well-being for individuals around the world.
References
Chang, A. Y. (2019, August 1). Chronic multimorbidity among older adults in rural South Africa. BMJ Global Health. https://doi.org/10.1136/bmjgh-2018-001386
Disang, M. D. R. W. (2021, March 22). Prevalence and patterns of chronic communicable and non-communicable diseases multimorbidity in sub-Saharan Africa: protocol for a systematic review | Published in the Journal of Global Health Reports. Prevalence and Patterns of Chronic Communicable and Non-Communicable Diseases Multimorbidity in Sub-Saharan Africa: Protocol for a Systematic Review. https://doi.org/10.29392/001c.21340
Goodman, R. A., Ling, S. M., Briss, P. A., Parrish, G. R., Salive, M. E., & Finke, B. S. (2015, December 28). Multimorbidity Patterns in the United States: Implications for Research and Clinical Practice. OUP Academic. https://doi.org/10.1093/gerona/glv199
King, D. E. (2018). Multimorbidity Trends in United States Adults, 1988–2014. PubMed. https://www.jabfm.org/content/31/4/503
Multiple morbidities as a global health challenge | The Academy of Medical Sciences. (2021). Multiple Morbidities as a Global Health Challenge. https://acmedsci.ac.uk/policy/policy-projects/multiple-morbidities-as-a-global-health-challenge
National health insurance policy in Nepal: challenges for implementation. (2015). PubMed Central (PMC). https://dx.doi.org/10.3402%2Fgha.v8.28763
News Medical. (2018, October 24). Multimorbidity Treatment Challenges. News-Medical.Net. https://www.news-medical.net/health/Multimorbidity-Treatment-Challenges.aspx
Overweight, obesity, and risk of cardiometabolic multimorbidity: pooled analysis of individual-level data for 813 adults from 16 cohort studies from the USA and Europe. (2017, June 1). ScienceDirect. https://doi.org/10.1016/S2468-2667(17)30074-9
Prevalence and correlates of Multimorbidity among older adults in rural Nepal: a cross sectional study. (2020, April 7). Research Square. https://doi.org/10.21203/rs.3.rs-19792/v1
Waschkau, A. (2019, February 27). Are big data analytics helpful in caring for multimorbid patients in general practice? - A scoping review. BMC Family Practice. https://doi.org/10.1186/s12875-019-0928-5
Yadav, U. N. (2021, February 1). Prevalence of non-communicable chronic conditions, multimorbidity and its correlates among older adults in rural Nepal: a cross-sectional study. BMJ Open. https://doi.org/10.1136/bmjopen-2020-041728
Images
Chang, A. Y. (2019, August 1). Chronic multimorbidity among older adults in rural South Africa. BMJ Global Health. https://doi.org/10.1136/bmjgh-2018-001386
Most prevalent multimorbidities in Nepal from a cross-sectional study by the Forum for Health Research and Development for 794 Nepalese adults. (2020). [Graph]. https://assets.researchsquare.com/files/rs-19792/v1/ed85e590-3c9b-4770-b15b-fb9bd9d57aa2.pdf?c=1631832768
World Population Review - Human Development Index. Human development index (HDI) by country. (n.d.). Retrieved October 28, 2021, from https://worldpopulationreview.com/country-rankings/hdi-by-country.